|
The JOURNAL of APPLIED RESEARCH In Clinical and Experimental Therapeutics |
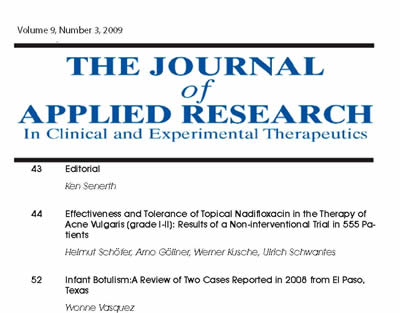 |
| Current Issue |
| Previous Issues |
| Reprint Information |
| Back to The Journal of Applied Research |
Endotracheal Tube Cuff Pressure Threshold for Prevention of Nosocomial Pneumonia
A Chendrasekhar, MD
G. A. Timberlake, MD
Trauma Services, Iowa Methodist Medical Center, Des Moines, Iowa
KEY WORDS: Nosocomial pneumonia, endotracheal tube, ventilator-associated subglotic secretions, glucose levels
Abstract
Ventilator-associated pneumonia (VAP) is commonly seen
as a complication in trauma patients. In patients with adult respiratory
distress syndrome (ARDS), the incidence of VAP can be as high as 70%.
Although much has been written about therapy, little has been written
about prevention by addressing etiology and pathology. A microaspiration-enabled,
high-volume, low-pressure cuffed endotracheal tube is a likely etiology
for early ventilator-associated pneumonia. Aspiration of subglottic
secretions has been shown to reduce the incidence of early ventilator-associated
pneumonia in intubated, mechanically ventilated patients. Most intensive-care
units use cuff pressure sufficient to prevent air leak in a retrograde
manner (usually no greater than 20 cm H2O).
The exact threshold beyond which subglottic secretions freely cross
the balloon barrier is unknown. We determined this threshold level by
a model using ex vivo porcine tracheas.
Introduction
Ventilator-associated pneumonia (VAP) is commonly seen as a complication in trauma patients. In trauma patients with multiple injuries undergoing mechanical ventilation, the incidence ranges from 22% to 44%.1,2 In patients with adult respiratory distress syndrome (ARDS), the incidence of VAP can be as high as 70%.3 Most of these VAPs seen in trauma patients are classified as early VAP. Although much has been written about the therapy of VAP, little has been written about the prevention of VAP by addressing etiology and pathology.
A microaspiration-enabled, high-volume, low-pressure cuffed endotracheal tube is a likely etiology for early ventilator-associated pneumonia.4 Aspiration of subglottic secretions has been shown to reduce the incidence of early ventilator-associated pneumonia in intubated, mechanically ventilated patients.5,6 In the original study evaluating continuous aspiration of subglottic secretions (CASS), the incidence of pneumonia was also related to the maintenance of threshold endotracheal tube (ETT) cuff pressure.5 Most intensive-care units use cuff pressure sufficient to prevent air leak in a retrograde manner (usually no greater than 20 cm H2O). The concern with increasing the cuff pressure beyond this threshold is that mucosal blood supply could be compromised and this could result in future subglottic stenosis.5
The exact threshold beyond which subglottic secretions freely cross the balloon barrier is unknown. We determined this threshold level by a model using ex vivo porcine tracheas.
Methods
This protocol was exempted from review by our Institutional Animal Care and Utilization Committee because we used ex vivo tracheas obtained from previously euthanized mixed-breed pigs, which were used for gynecologic experimental protocols. Tracheal segments measuring at least 3 cm in length were removed from 10 adult swine used for ex vivo testing. The tracheas were removed from the pigs within 30 minutes of euthanasia, covered with saline-soaked gauze, and placed into zip-lock plastic bags. The tracheal segments were then brought to our lab site where the experimental protocol was carried out.
Experimental Protocol
The tracheal segment was held in place by using a simple laboratory clamp. The tracheal segment was then intubated with a tracheostomy tube. Ventilatory motion was simulated for 2 minutes with approximately 30 breaths with associated movements up and down the tracheal segment of approximately 0.5 cm. Five milliliters of concentrated glucose solution was placed above the ETT cuff and the glucose levels below the cuff were tested by swabbing the wall of the trachea below the ETT cuff at sequential cuff pressures. The swab was then applied to a glucometer to assess glucose levels. The fluid above the ETT cuff was suctioned out and an additional 5 mL of glucose solution was placed above the cuff, and the process of ventilation at the new cuff pressure was initiated once again. Each glucose value for a particular tracheal segment and particular cuff pressure was checked 3 times for internal consistency and then averaged. The cuff pressures were lowered from 50 cm H2O to 5 cm H2O in decrements of 5 cm H2O. Leak threshold was defined as glucose level greater than 80 mg/dL. Glucose determination was performed by using a commercially available glucometer (Fig. 1). The average glucose value (from 3 readings) for each tracheal segment at a given cuff pressure was then averaged with the same cuff pressure value for each of the 10 tracheal segments. The average data were then plotted over the entire range of cuff pressures to see if a step-off value was present. Using this plot and the cutoff value in glucose of 80 mg/dL, an average cuff pressure needed to maintain secretions above the cuff was calculated.
Results
The tracheal segments tested all tolerated the endotracheal tube placement and ventilatory simulation without any signs of tissue disruption. The averaged glucose levels at each cuff pressure were plotted (Fig. 2). The average ETT cuff pressure required to maintain secretions above the cuff was 29.5 ± 3.2 cm H2O (mean ± standard error of mean).
Discussion
Ventilator-associated pneumonia is a common complication in trauma patients. The theory regarding microaspiration supports the notion that any bacteria accumulates above the cuff. Microaspiration-enabled, high-volume, low-pressure cuffed endotracheal tubes have been suggested as a possible etiology of early ventilator-associated pneumonia.1,5,6 Stated briefly, secretions build up above the cuff of an endotracheal tube. Positive pressure ventilation does result in some upward and downward movement of the endotracheal tube during the course of the respiratory cycle. This results in the aerosolization of the bacteria present in the above ETT cuff (subglottic) secretions. The bacteria lodge in the distal tracheobronchial tree and develop in some patients into a VAP.5,6
Continuous aspiration
of subglottic secretions has been shown as a method of reducing the
incidence of early VAP.5,6 In the original study evaluating CASS, the
incidence of pneumonia was related per the authors to the maintenance
of a threshold ETT cuff pressure of 20 cm H2O.5 The authors did not elaborate on the issue of
threshold at or above which seepage could be minimized. We felt that
this information would be beneficial because reduction of this seepage
could indeed prevent VAP. This is the first study to assess the threshold
pressure required to keep secretions above the ETT cuff within a trachea.
We found that we were able to take fresh cadaveric tracheal segments
and subject them to the rigors of our experimental protocol without
getting any disruption of the segments. We also found that the seepage
rate from above to below the cuff at each pressure level was consistent
not only within the same tracheal segment, but also consistent between
tracheal segments. Our experimental protocol showed that a mean ETT
cuff pressure at 29.5 cm H2O
or above maintained the secretions above the cuff. Below this level,
seepage of subglottic secretions is evident as documented by an increased
glucose level below the ETT cuff.
The standard protocol followed by respiratory therapists is to increase the cuff pressure until a minimal cuff leak is noted. In adult respiratory distress syndrome in which plateau pressures and peak pressures exceed 30 cm H2O, the cuff pressures required to keep the leak to a minimal level will be at or above our threshold of 29.5 cm H2O. As far as tracheal wall blood supply depletion, clinical tracheal stenosis is not seen in patients in whom ARDS has led to using cuff pressures in excess of 30 cm H2O. This could also explain why different and more resistant bacteria are noted later in trauma patients with ARDS as compared with early ventilator pneumonias seen in these patients.5,6 It could be that the mechanism of acquiring the later pneumonia might not be related to the seepage phenomenon.
The shortcomings of our study were that we used an ex vivo model, which meant that we could not simulate the blowback, which is usually seen around the ETT cuff in patients on positive pressure ventilation. The blowback, which might be noted as an air leak, could reduce the incidence of seepage at a given level of cuff pressure. Clearly oropharyngeal secretions are usually thicker than water alone; the increased viscosity could also reduce the incidence of seepage and microaspiration.
Our study does, however,
provide some insights into cuff pressure management in mechanically
ventilated patients. For example, the incidence of ventilator-associated
pneumonia is approximately 70% in patients with ARDS.3 With plateau
pressures and peak pressures well in excess of 30 cm H2O,
the utility of a cuff pressure greater than 30 cm H2O might be appropriate and might not be deleterious
to tracheal wall blood flow. Also, if the subglottic secretions are
controlled from seepage, it could improve outcome with regard to VAP.
Clearly, more in vivo basic science and clinical studies are needed
to assess the threshold of seepage versus the threshold where tracheal
blood supply is compromised. Such studies will better delineate these
issues.
References
1. Rello J, Ausina V, Castella J, et al: Nosocomial respiratory tract infections in multiple trauma patients: influence of level of consciousness with implications for therapy. Chest 102:525, 1992.
2. Rodriquez JL, Gibbons KJ, Bitzer LG, et al: Pneumonia: Incidence, risk factors, and outcome in injured patients. J Trauma 31:907, 1991.
3. Niederman
MS, Fein AM: Sepsis syndrome, the adult respiratory distress syndrome
and nosocomial pneumonia. Clin Chest Med
11:633, 1990.
4. Craven DE, Steger KA, Barber TW: Preventing nosocomial pneumonia: state of the art & perspectives for the 1990's. Am J Med 91(suppl 3B): 44S, 1991.
5. Rello J, Sonora R, Jubert P, et al: Pneumonia in intubated patients: role of respiratory airway care. Am J Respir Crit Care Med 154:111, 1996.
6.
Valles J, Artigas A, Rello J, et al: Continuous
aspiration of subglottic secretions in preventing ventilator associated
pneumonia. Ann Intern
Med 122:179, 1995.
Figure
1. Glucose determination
was performed using a commercially available glucometer.
Figure 2. Averaged glucose levels
at each cuff pressure.
©2000-2013. All Rights Reserved. Veterinary Solutions LLC
2Checkout.com is an authorized retailer for The
Journal of Applied Research