|
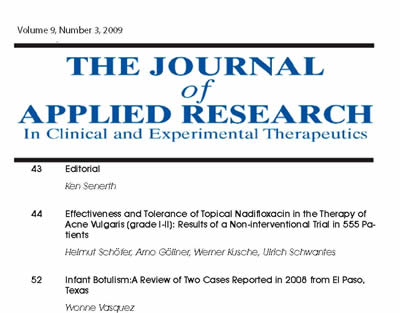
The JOURNAL of APPLIED RESEARCH In Clinical and Experimental Therapeutics |
 |
| Current Issue |
| Previous Issues |
| Reprint Information |
| Back to The Journal of Applied Research |
Blood Pressure, Weight, and Cholesterol: A Report of the Program on the Surgical Control of the Hyperlipidemias (POSCH)
James R. Boen, PhD
Phuong A. Nguyen, BA*
John P. Matts, PhD
Division
of Biostatistics in the
University of
abstract
Objective: To examine the blood pressure (BP), weight, and cholesterol data from the Program on the Surgical Control of the Hyperlipidemias (POSCH). Blood pressure (BP) reductions have been attributed to extra-lipid effects of statin drugs. In POSCH, no statin drugs were used and marked lipid reduction was achieved by partial ileal bypass operation.
Methods: Plasma total and low-density lipoprotein (LDL) cholesterol, BP, and body weight (as body mass index [BMI]) in POSCH patients at baseline and at 5-years after randomization were compared.
Results: There were no statistically significant differences in mean systolic or diastolic BP between the control and intervention groups at baseline. At 5 years, however, statistically significant (P <0.0005) differences in mean systolic and diastolic BP were found between the groups. Similarly, the differences between the groups in BMI and plasma total and LDL-cholesterol were not statistically significant at baseline, but were at 5 years (P <0.0001). By multivariate regression analyses, consistent, statistically significantly relationships were found between BMI and BP (P <0.0001). In addition, for systolic BP, in the entire POSCH population (n = 838), a statistically significant relationship was found on regression analysis for the plasma total cholesterol (P <0.013).
Conclusion: POSCH is the only major lipid/atherosclerosis trial to establish a relationship between cholesterol reduction and BP reduction without the need to implicate statin drugs extra-lipid effects.
Introduction
Anecdotal reports have come from the lipid/atherosclerosis trials of incidental reductions in blood pressure (BP) in the intervention groups.15 For the most part, those trials used pharmaceutical agents, predominantly statin drugs with possible secondary endothelial effects, to achieve lipid modification. These findings have led us to examine the data from the Program on the Surgical Control of the Hyperlipidemias (POSCH) trial, in which marked lipid reduction was achieved by partial ileal bypass operation and no statin or other lipid-lowering pharmaceutical agent was used.
Methods
POSCH Overview
POSCH was a multiclinic, randomized, prospective, secondary intervention trial designed to ascertain whether the effective reduction of plasma total cholesterol and low-density lipoprotein (LDL) cholesterol levels and the increase in the plasma high-density lipoprotein (HDL) cholesterol levels induced by partial ileal bypass operation had a favorable impact on overall mortality and on the mortality and morbidity attributable to atherosclerotic coronary heart disease (ACHD). POSCH used both clinical and arteriographic end points, the first atherosclerosis intervention trial to correlate changes observed on sequential coronary arteriograms with clinical atherosclerotic events.
From 1975 through 1983, a total of 838 survivors of a single myocardial infarction, documented by electrocardiograms and changes in enzyme values, were entered into POSCH. The patients, both men and women, were between the ages of 30 and 64 years. To be eligible for the trial, they had to have a plasma cholesterol level greater than 5.69 mmol/L (220 mg/dL), or greater than 5.17 mmol/L (200 mg/dL) if the LDL cholesterol level was in excess of 3.62 mmol/L (140 mg/dL). Patients were randomly assigned either to treatment with diet instruction only (n = 417, control group) or to diet intervention plus partial ileal bypass surgery (n = 421, intervention group). The formal trial ended July 19, 1990, with a mean patient follow-up of 9.7 years (range, 7.014.8 y). The initial report of the POSCH data was the first affirmation of the lipid/atherosclerosis hypothesis and demonstrable ACHD benefits by cholesterol reduction.6 In 1998, the POSCH 5-year posttrial follow-up report was published.7
Partial ileal bypass effected a 23.3% reduction in total plasma cholesterol, a 37.7% reduction in LDL-cholesterol, and a 4.3% increase in HDL-cholesterol at 5 years after randomization in the intervention group compared with the control group. These findings were accompanied by a 35.0% lower mortality rate from ACHD combined with confirmed nonfatal myocardial infarction (P <0.001), a 36.0% lower overall mortality rate in the intervention subgroup with a left ventricular ejection fraction of 50% or more (P = 0.05), a 60.1% lower incidence of coronary artery bypass grafting and percutaneous transluminal coronary angioplasty (P <0.001), and a consistently lower rate of disease progression on comparison of the baseline coronary arteriograms with those obtained at 3, 5, 7, and 10 years after randomization in the intervention group (P <0.001 for each time interval compared with baseline).6 At 5 years after the formal trial ended (mean follow-up, 14.7 y; range, 12.220 y), statistical significance was obtained for differences in overall mortality (P = 0.049), ACHD mortality (P = 0.03), and the onset of clinical peripheral vascular disease (P = 0.02).7 No statistically significant differences were found between the control and intervention groups for cerebrovascular events, non-ACHD mortality, and cancer.
Study Design
Most of the potentially confounding major risk factors for atherosclerosis were criteria for exclusion from the POSCH trial, including hypertension (defined as a systolic BP ³180 mm Hg or a diastolic BP ³105 mm Hg). BP measurements were determined at baseline, before randomization, 3 months after randomization, and at every subsequent clinic visit (annually during the first 5 y, then 1 visit at 7 or 10 y); they were discontinued in 1990. In addition to BP exclusion criteria, patients with a body weight 40% above the ideal weight and/or the presence of diabetes mellitus were excluded from this trial. For the current analysis, we compared baseline and 5 years postrandomization values for plasma total and LDL-cholesterol, BP, and body weight as body mass index (BMI = wt in kg/ht in m2). Of the 417 control group patients at baseline, 406 had 5-year follow-up determinations; of the 421 intervention group patients, 410 had 5-year follow-up determinations.
Statistical Analysis
Results are expressed as means ± the standard deviation (SD). A t test was used to compare the baseline and 5-year values. Multivariate regression analyses with BP as the dependent variable were performed with the following variables: age, gender, plasma total cholesterol, plasma LDL-cholesterol, BMI, systolic BP, and diastolic BP. Systolic BP and diastolic BP were examined separately. Plasma total cholesterol and plasma LDL-cholesterol were not simultaneously included in the same model. The values used for plasma total cholesterol, plasma LDL-cholesterol, systolic BP, diastolic BP, and BMI were the average of the annual follow-up values over 5 years. A two-sided P-value less than 0.05 was considered statistically significant.
Results
There were no statistically significant differences in mean systolic or diastolic BP between the control and the intervention groups at baseline. At 5 years follow-up, however, statistically significant (P <0.0005) differences in mean systolic and diastolic BP were found between the groups (Table 1). Similarly, the differences between the groups in the BMI and the plasma total and LDL-cholesterol were not statistically significant at baseline, but were at 5 years (P <0.0001; Table 1). For systolic BP, the change (control group intervention group) from a 0.6 mm Hg difference at baseline to a 3.0 mm Hg difference at 5 years was primarily the result of an increase in systolic BP in the control group and of a mild decrease in the intervention group with age.
In our multivariate regression analyses, BMI was consistently statistically significantly related to both systolic and diastolic BP (P <0.0001) and had the strongest relationship with the alterable variables of BMI, plasma total cholesterol, and plasma LDL cholesterol. For systolic BP, in the entire POSCH population (n = 838), a statistically significant relationship was found on regression analysis for the plasma total cholesterol (P <0.013; Table 2). This relationship is expressed as an equation in Table 3. A statistically significant relationship was not found for systolic BP and plasma LDL cholesterol. Neither of the lipid variables was statistically significant using diastolic BP for a dependent variable. Age was significantly related to systolic BP (P <0.001) but not to diastolic BP. Being male was significantly related to higher diastolic BP (P = 0.001) but not to systolic BP.
Discussion
The tripartite relationship among BP, weight, and plasma cholesterol is well known; the precise mechanisms involved are less clearly defined. Well over 50 studies in the literature suggest a positive association between BP and body weight, including the INTERSALT study of 10,079 men and women.8 In INTERSALT, a 3.0 mm Hg difference in systolic BP and a 2.2 mm Hg difference in diastolic BP were associated with a 10-kg difference in body weight. In the vast bariatric surgery literature, all studies reporting BP changes confirm a marked lowering of the BP after weight loss.9,10 The mechanisms related to a decrease in BP after weight loss include a reduction in vascular resistance, total blood volume, and cardiac output; an improvement in insulin resistance; a reduction in sympathetic nervous system activity; and suppression of the activity of the renin angiotensin aldosterone system.11-15
Increased plasma total cholesterol levels are associated, in both men and women, with increases in body weight,1618 especially at levels of BMI >25.19,20 Cross-sectional studies suggest that LDL-cholesterol levels are higher, by 0.26 to 0.52 mmol/L (10=20 mg/dL), in relation to a 10-unit difference in BMI for BMI levels of 20 to 30.19,20 Again, the bariatric surgery literature is replete with affirmations that reductions in total plasma cholesterol and LDL-cholesterol are associated with weight loss.9,10 With respect to mechanisms, correction of the hypoinsulinemia and hyperglycemia in type I diabetics and of the peripheral insulin resistance and hyperglycemia in type II diabetics is associated with a normalization of the lipid profile.21,22
When it comes to the relationship of BP and the plasma lipids, the data are scarcer and less precise. A strong correlation between high plasma cholesterol concentrations and impaired endothelium-dependent vascular relaxation has been demonstrated.2329 Furthermore, in experimental studies, this vascular dysfunction has been associated with biosynthesis of nitric oxide, plasma renin activity, calcium influx, and elaboration of vasoconstriction autocoids.3035 Clinically, diastolic BP changes during gentle exercise are positively associated with plasma concentrations of plasma total cholesterol.36
Specific studies of the effect of statin drugs on BP have shown BP reductions in patients on ACE inhibitors,37,38 no BP reductions in patients on ACE inhibitors,39 and equivocal results in patients on ACE inhibitors.40 With respect to the mechanism of statins, experimental studies suggest that HMG CoA-reductase inhibitors enhance endothelial function independent of their lipid-lowering effects,41 and that cholesterol-lowering treatment with statins reverses the elevated BP response to angiotensin II and downregulates angiotensin II type 1 receptor activity.42
In POSCH, the intervention modality of partial ileal bypass resulted in a statistically significant reduction in overall mortality, as well as in ACHD mortality and morbidity, in association with a marked lowering of total plasma cholesterol and LDL-cholesterol.6,7 In addition, the intervention group at 5 years had significantly lower body weights and significantly lower systolic and diastolic BP.
Why was the BP lowered
in POSCH? Certainly, the BP reduction was not the result of the extra-lipid
effects of statin or other drugs, because lipid reduction in POSCH
was brought about by a surgical procedure. One possible cause for
the BP reduction is the reduction in body weight. Other reasons might
be found in the mechanisms previously stated in this article. Finally,
the BP reduction might have been related to an increase in oxygen
transport. Hypercholesterolemia has been shown to impair the rate
of oxygen desaturation,43 which, in turn, may increase BP as mediated
by carotid body receptors.44 Thus, the POSCH cholesterol reduction
might have increased the oxygen desaturation rate, ie, increased oxygen
transport and
thereby lowered BP.
In summary, POSCH was the first randomized clinical trial to prove the lipid/atherosclerosis hypothesis and the first major trial to show a lowering of the BP concomitant with marked reductions of plasma total cholesterol and LDL-cholesterol. POSCH is the only major lipid/atherosclerosis trial to establish this relationship between cholesterol reduction and BP reduction without the need to implicate extra-lipid effects of statin or other drugs.
Acknowledgments
This study was supported
by grants RO1-HL-15265 and RO1-HL-49522 from the National Heart, Lung,
and Blood Institute, Bethesda, Maryland, and a special grant from
the Department of Surgery and the Dean of the Medical School of the
University of Minnesota, Minneapolis, Minnesota.
References
1. Committee of Principal Investigators: A co-operative trial in the primary prevention of ischaemic heart disease using clofibrate. Br Heart J 40:10691118, 1978.
2. Morgan T, Anderson A, McDonald P, Hopper J, Macaskill G: Simvastatin in the treatment of hypercholesterolaemia in patients with essential hypertension. J Hypertens 8(suppl):S2530, 1990.
3. Bradford RH, Shear CL, Chremos AN, et al: Expanded clinical evaluation of lovastatin (EXCEL) study results, I: efficacy in modifying plasma lipoproteins and adverse event profile in 8,245 patients with moderate hypercholesterolemia. Arch Intern Med 515:4349, 1991.
4. Arntzenius AC, Kromhout D, Barth JD, et al: Diet, lipoproteins, and the progression of atherosclerosis. The Leiden Intervention Trial. N Engl J Med 312:805811, 1985.
5. Duffield RGM, Miller NE, Brunt JNH, et al: Treatment of hyperlipidemia retards progression of symptomatic femoral atherosclerosis. Lancet 2:639642, 1983.
6. Buchwald H, Varco RL, Matts JP, et al: Effect of partial ileal bypass surgery on mortality and morbidity from coronary heart disease in patients with hypercholesterolemia. Report of the Program on the Surgical Control of the Hyperlipidemias (POSCH). N Engl J Med 323:946955, 1990.
7. Buchwald H, Campos CT, Varco RL, et al: Effective lipid modification by partial ileal bypass reduced long-term coronary heart disease mortality and morbidity: five-year posttrial follow-up report from the POSCH. Arch Intern Med 158:12531261, 1998.
8. Dyer AR, Elliott P: The INTERSALT study: relations of body mass index to blood pressure. J Human Hypertension 3:299308, 1989.
9. Deitel M, ed. Surgery for the Morbidly Obese Patient. Philadelphia: Lea & Febiger; 1989.
10. Deitel M, Cowan SGM Jr, eds. Update: Surgery for the Morbidly Obese Patient. Toronto: FD-Communications Inc, 2000.
11. Reisin E, Frolich ED, Messerli FH, et al: Cardiovascular changes after weight reduction in obesity hypertension. Ann Intern Med 98:315319, 1983.
12. Tuck ML, Sowers J, Dornfield L, Kledzik G, Maxwell M: The effect of weight reduction on blood pressure plasma renin activity, and plasma aldosterone levels in obese patients. N Engl J Med 304:930933, 1981.
13. Rocchini AP, Key J, Bondie D, et al: The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N Engl J Med 321:580585, 1989.
14. Landsberg L, Krieger DR: Obesity, metabolism, and the sympathetic nervous system. Am J Hypertens 2:125S132S, 1989.
15. Jacobs DB, Sowers JR, Hmeidan A, et al: Effects of weight reduction on cellular cation metabolism and vascular resistance. Hypertension 21:308314,1993.
16. Ashley FW Jr, Kannel WB: Relation of weight change
to changes in atherogenic traits: the Framingham Study. J Chron Dis
27:103114, 1974.
17. Hershcopf RJ, Elahi D, Andres R, et al: Longitudinal changes in serum cholesterol in man: an epidemiologic search for an etiology. J Chron Dis 35:101104, 1982.
18. Shekelle RB, Shryock AM, Paul O, et al: Diet, serum cholesterol, and death from coronary heart disease. The Western Electric study. N Engl J Med 304:6570, 1981.
19. Denke MA, Sempos CT, Grundy SM: Excess body weight. An underrecognized contributor to high blood cholesterol levels in white American men. Arch Intern Med 153:10931103, 1993.
20. Denke MA, Sempos CT, Grundy SM: Excess body weight. An underrecognized contributor to dyslipidemia in white American women. Arch Intern Med 154:401410, 1994.
21. Unger RH, Foster DW: Diabetes Mellitus. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR, eds. Williams Textbook of Endocrinology. Philadelphia: WB Saunders Co; 1998:9731059.
22. Mahley RW, Weisgraber KH, Farese RV Jr: Disorders of lipid metabolism. In: Wilson JD, Foster DW, Kronenberg HM, Larsen PR, eds. Williams Textbook of Endocrinology. Philadelphia: WB Saunders Co; 1998:10991153.
23. Lewis TV, Cooper BA, Dart AM, Chin-Dusting JP: Responses to endothelium-dependent agonists in subcutaneous arteries excised from hypercholesterolaemic men. Br J Pharmacol 124:222228, 1998.
24. Stroes E, de Bruin T, de Valk H, et al: No activity in familial combined hyperlipidemia: potential role of cholesterol remnants. Cardiovasc Res 36:445452, 1997.
25. Stroes ES, Koomans HA, de Bruin TW, Rabelink TJ: Vascular function in the forearm of hypercholesterolaemic patients off and on lipid-lowering medication. Lancet 346:467471, 1995.
26. Creager MA, Cooke JP, Mendelsohn ME, et al: Impaired vasodilation of forearm resistance vessels in hypercholesterolemic humans. J Clin Invest 86:228234, 1990.
27. Chowienczyk PJ, Watts GF, Cockcroft JR, Ritter JM: Impaired endothelium-dependent vasodilation of forearm resistance vessels in hypercholesterolaemia. Lancet 340:14301432, 1992.
28. Casino PR, Kilcoyne CM, Quyyimi AA, Hoeg JM, Panza JA: The role of nitric oxide in endothelium-dependent vasodilation of hypercholesterolemic patients. Circulation 88:25412547, 1993.
29. Goode GD, Heagerty AM: In vitro responses of human peripheral small arteries in hypercholesterolemia and effects of therapy. Circulation 91:28982903, 1995.
30. Vidal F, Colome C, Martinez-Gonzalez J, Badimon L: Atherogenic concentrations of native low-density lipoproteins down-regulate nitric-oxide-synthase mRNA and protein levels in endothelial cells. Eur J Biochem 252:378384, 1998.
31. Kotchen TA, Talwalker RT: Increased enzymatic activity of renin and hyperlipidemia. Am J Physiol 240:E60E64, 1981.
32. Gleason MM, Medow MS, Tulenko TN: Excess membrane cholesterol alters calcium movements, cytosolic calcium levels, and membrane fluidity in arterial smooth muscle cells. Circ Res 69:216227, 1991.
33. Rubattu S, Volpe M, Enea I, et al: Influence of hypercholesterolemia on adrenal steroid metabolism and electrolyte balance in spontaneously hypertensive rats. Endocrinology 133:20152021, 1993.
34. Mangiafico RA, Malatino LS, Santonocito M, et al: Raised plasma endothelin-1 concentrations in patients with primary hypercholesterolemia without evidence of atherosclerosis. Int Angiol 15:240244, 1996.
35. Lerman A, Webster MW, Chesebro JH, et al: Circulating and tissue endothelin immunoreactivity in hypercholesterolemic pigs. Circulation 88:29232928, 1993.
36. Brett SE, Ritter JM, Chowienczyk PJ: Diastolic blood pressure changes during exercise positively correlate with serum cholesterol and insulin resistance. Circulation 101:611615, 2000.
37. Sposito AC, Mansur EP, Coelho OR, Nicolau JC, Ramires JA: Additional reduction in blood pressure after cholesterol-lowering treatment by statins (Lovastatin or Pravastatin) in hypercholesterolemic patients using angiotensin-converting enzyme inhibitors (Enalapril or Lisinopril). Am J Cardiol 83:14971499, 1999.
38. Borghi C, Prandin MG, Costa FV, et al: Use of statins and blood pressure control in treated hypertensive patients with hypercholesterolemia. J Cardiovasc Pharmacol 35:549555, 2000.
39. OCallaghan CJ, Krum H, Conway EL, et al: Short term effects of pravastatin on blood pressure in hypercholesterolemic hypertensive patients. Blood Pressure 3:404406, 1994.
40. Glorioso N, Troffa C, Filigheddu F, et al: Effect of the HMG-CoA reductase inhibitors on blood pressure in patients with essential hypertension and primary hypercholesterolemia. Hypertension 34:12811286, 1999.
41. Jarvisalo MJ, Toikka JO, Vasankari T, et al: HMG CoA reductase inhibitors are related to improved systemic endothelial function in coronary artery disease. Atherosclerosis 147:237242, 1999.
42. Nickenig G, Baumer AT, Temur Y, et al: Statin-sensitive dysregulated AT1 receptor function and density in hypercholesterolemic men. Circulation 100:21312134, 1999.
43. Buchwald H, Menchaca HJ, Michalek VN, et al: Plasma cholesterol: a controlling factor in RBC O2 release and cellular O2 availability, report of 100 patients. J Am Coll Surg 191:490497, 2000.
44.
Donnelly DF: Developmental aspects of oxygen sensing by the
carotid body. J Appl Physiol 88:22962301, 2000.
Table 1. Blood Pressure, Body Mass Index, and Plasma
Total Cholesterol
Baseline
Control Intervention t
Value P Value
Systolic BP 121.6 ± 14.0 120.8±14.5 .726 0.47
Diastolic BP 79.0 ± 9.3 78.7 ± 9.0 .306 0.76
BMI 27.0 ± 3.1 27.1 ± 2.9 .209 0.83
Plasma 250.58 ±
35.19 251.36 ± 37.12 .267 0.79
cholesterol
5-Year
Follow-Up
Baseline
Control Intervention t
Value P Value
Systolic BP 123.3 ± 12.2 120.3 ± 11.5 3.58 <0.0005
Diastolic BP 79.9 ± 7.2 78.1 ± 6.8 3.57 <0.0005
BMI 27.5 ± 3.6 25.8 ± 3.2 7.35 <0.0001
Plasma 237.43 ±
34.42 161.25 ± 35.19 21.39 <0.0001
cholesterol
BP,
blood pressure (mm Hg); BMI, body mass index (kg/m2); plasma cholesterol
as ±
standard deviation in mg/dL.
Table 2. Multivariate Regression Analysis for Systolic
Blood Pressure
Standard
Variable Coefficient Error P Value
Intercept 77.13 4.90 0.0001
Age (y) 0.41 0.53 0.0001
Gender -0.70 1.40 0.6150
BMI 5-y 0.75 0.12 0.0001
TC 5-y 0.02 0.01 0.0130
BMI,
body mass index (kg/m2); TC, plasma total cholesterol.
Table 3. Multivariate Regression Analysis for Systolic
Blood Pressure
Systolic BP = 77 + .41 age (in years) .70 gender (1 male, 2 female) +.75 BMI + 0.02 TC (in mg/dL)
BP, blood pressure; BMI, body mass index (kg/m2); TC = plasma total cholesterol.
©2000-2013. All Rights Reserved. Veterinary Solutions LLC
2Checkout.com is an authorized retailer for The
Journal of Applied Research